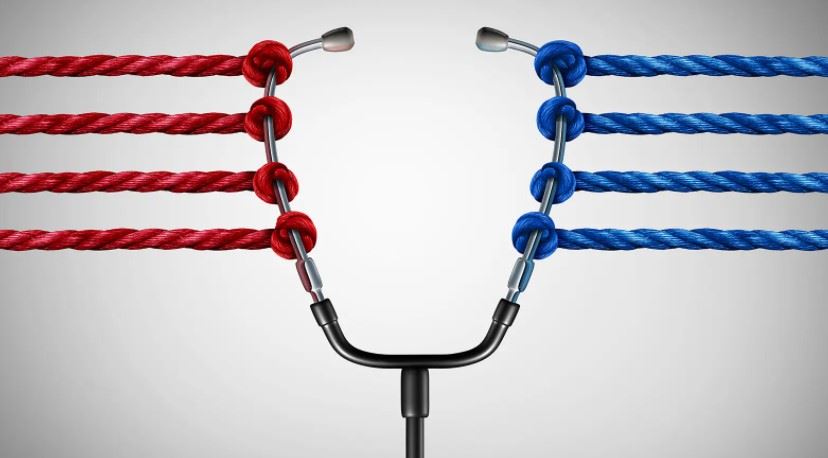
 Democratic and Republican House members appeared as far apart as ever Tuesday on the issue of the best way to achieve universal healthcare coverage in the U.S.
Democratic and Republican House members appeared as far apart as ever Tuesday on the issue of the best way to achieve universal healthcare coverage in the U.S.
"Republicans are serious on this committee about trying to solve the healthcare problems we have in America, but bigger government and government-run healthcare is not the solution to the problem," said Rep. James Comer (R-Ky.), ranking member of the House Oversight and Reform Committee, which held a hearing on "Examining Pathways to Universal Health Coverage."
For a large number of Democratic committee members, however, government-run healthcare -- such as through a "Medicare for All" program -- was exactly the answer. "For my colleagues on this committee, you have a choice in front of you today," said Rep. Cori Bush (D-Mo.). "It's a choice to save lives or a choice to let people die ... I came to Congress because 'Medicare for All,' it's not a choice for me. It's a moral imperative."
Contrary Presentations of Facts
Viewers trying to figure out what the facts were on the issue would have been hard-pressed to do so. Would a government-run system cost more money? Absolutely, according to committee member Rep. Andrew Clyde (R-Ga.). He cited an Urban Institute report saying that a single-payer healthcare plan that would cover all residents -- including undocumented immigrants -- would cost the federal government $34 trillion over 10 years.
No, it wouldn't cost more money -- instead, it would save money, according to committee chair Rep. Carolyn Maloney (D-N.Y.). "I would like to submit for the record a study from the University of California San Francisco, which analyzed 22 single-payer proposals and found that every single one would result in long-term financial savings," she said. "If my Republican colleagues were really worried about inflation, they would support policies that bring down healthcare costs, instead of voting 60 times against the Affordable Care Act healthcare plan that has expanded healthcare to 30 million Americans."
One thing that committee members and witnesses agreed on: the current system is not working very well. "The U.S. system is completely broken," said Jeffrey Sachs, PhD, director of the Columbia University Center for Sustainable Development. "We are spending a fortune -- unlike every other country -- and we're getting worse outcomes. This is what needs to be understood beyond the ideology, beyond the anecdotes."
"There's no question Americans remain frustrated with the current healthcare system," said Grace-Marie Turner, president of the Galen Institute, a right-leaning think tank in Paeonian Springs, Virginia. "But the more government gets involved, the more that we see the health sector is forced to comply with countless rules and regulations rather than innovating to respond to more choices of more affordable care and coverage for patients ... 'Medicare for All' would take us further toward government control of our health sector, with fewer choices."
Patient Stories
The committee heard from a panel of witnesses who described their challenges in getting healthcare. One was ALS activist Ady Barkan, JD. Three years ago, "I had to decide whether to get a tracheostomy ... to compensate for my failing diaphragm," Barkan said. "But I didn't know how I would be able to pay for the care that would allow me to stay alive. My insurance had already denied me a ventilator, stating that it was experimental. And then 2 weeks after that, they rejected access to an FDA-approved ALS drug."
Barkan's insurer also initially denied him home care, but "we eventually secured 24-hour home care after suing my health insurance company in federal court," he added. "Home care has been life-changing, allowing me to participate in my family's life in ways I thought were no longer possible for me."
"It is time for America to guarantee comprehensive, affordable healthcare for all. The best way to do that is by enacting 'Medicare for All,'" he concluded.
But Chris Briggs, public affairs counsel to the Independent Institute, an Oakland, California-based right-leaning think tank, had a different opinion of government-run healthcare. Prior to the Affordable Care Act, "the private marketplace consistently and reliably had offered us a wide variety of inexpensive plans that covered specialist care, even out of state," said Briggs, who lives in Northern Virginia and buys his own health insurance. However, "after the ACA went into effect, [whatever] that was left were increasingly costly plans with fewer benefits, including fewer doctors and fewer hospitals ... We were and still are to this day basically restricted to medical facilities within a short radius of our zip code."
This became an issue after his young daughter was diagnosed with leukemia, and Briggs and his wife wanted her to be treated at Johns Hopkins; their insurer said it would not cover that. "The situation was made all the more painful by swelling premiums, as well as by skyrocketing deductibles," he said. "Maximum out-of-pocket expenses can go as high as $16,500, as it has been for my family."
"Bad ideas don't get better just because you make them bigger," said Briggs. "We must prohibit the government -- that is to say, all of you -- from further interfering in the acquisition by private citizens of their preferred medical care. And we do that by repealing the ACA and placing back into the hands of Americans real, actuarially sound, automatically renewable insurance products created to meet individual needs."
Effects on Vulnerable Populations
Uché Blackstock, MD, an emergency physician in New York City, discussed her experience working in communities where many patients were uninsured or underinsured. "Lack of access to healthcare is one of the primary social determinants of health," she said.
"I can never forget the 40-year-old Black man with a history of high blood pressure, who came into my ER unconscious on a stretcher after he collapsed at home in front of his family," Blackstock continued. "The paramedics were performing CPR on him. The CT scan of his head showed a brain bleed, a complication of untreated high blood pressure. He had been unable to afford to pay out of pocket for his blood pressure medication since he lost a job a year prior, and as a result, his health insurance ... Now is the time to protect our most vulnerable and underserved communities and identify a pathway to ensuring universal healthcare for all Americans."
But Turner suggested a different approach. "Rather than dramatically expanding the role of government through new or expanded taxpayer-supported programs, I believe we need targeted approaches to address the specific needs of those who are uninsured or underinsured, especially focusing on those in marginalized communities," she said. "'Medicare for All' would restrict access to new medicines and treatments, lead to dramatic increases in federal spending, and really turn back the clock on innovations in personalized care."
Joyce Frieden oversees MedPage Today’s Washington coverage, including stories about Congress, the White House, the Supreme Court, healthcare trade associations, and federal agencies. She has 35 years of experience covering health policy.
###